New Health Advisory for Dengue Fever
Young Ju, Ph.D.
On June 25, 2024, the Centers for Disease Control and Prevention (CDC) issued a Health Advisory for Increased risk of dengue virus (DENV) infections in the U.S. (1)
The CDC issue different message types through their Health Alert Network:
Health Alerts convey the highest level of importance about a public health incident and require immediate action or attention
Health Advisories provide important information for a public health incident but may not require immediate action.
Health Updates provide updated information regarding a public health incident and are unlikely to require immediate action.
Info Services provide general information that is not necessarily related to an immediate public health threat.
If you want to stay informed, you can sign up for Health Alert Network email updates at: (https://emergency.cdc.gov/han/index.asp).
Dengue Fever (2, 3, 4)
Dengue fever is a mosquito-borne disease of which there are four serotypes (DENV 1-4). Scientists hypothesize that it evolved in nonhuman primates and jumped to humans in Africa or Southeast Asia between 500 and 1000 years ago (5). Not all mosquitoes spread it; almost all cases are transmitted through the Aedes species mosquitoes (mainly Aedes aegypti and Aedes albopictus). As the primary carriers, Aedes mosquitoes have specific cellular receptors and biological pathways that allow the virus to be transmitted to uninfected individuals through a bite; it is not directly transmitted from person to person except through blood transfusion, but humans are the primary hosts.
In general, infection with one serotype of DENV induces life-long protection against infection from the same serotype but not against the other three serotypes. Approximately 1 in 20 patients with dengue progress to develop severe dengue, a life-threatening disease. A pregnant woman infected near the time of birth can pass the virus to the baby through contact with mother’s blood during birth. A lactating woman with dengue can pass the virus through breast milk.
Dengue Fever Situation (2, 3)
In general, dengue fever is most common in tropical areas such as the Caribbean, Latin America, Southeast Asia, Africa, and the Pacific Islands. Dengue is uncommon in most of the U.S., except in six US territories classified as areas with frequent or continuous dengue transmission: Puerto Rico, Guam, American Samoa, the US Virgin Islands, the Federated States of Micronesia, the Republic of Marshall Islands, and the Republic of Palau.
In 2024, global reported dengue cases are the highest on record, particularly in the Americas. From Jan 1 - Jun 24, 2024, 43 countries in the Americas reported more than 9.7 million dengue cases–more than double the 4.6 million reported cases in all of 2023. A higher number of dengue cases have also been identified among U.S. travelers; it is speculated that they are visiting areas where dengue is more common and returning home where mosquitoes could spread it. It’s possible that either infected travelers can spread it through mosquito bites or travelers can unintentionally bring infected mosquitoes with them. In March 2024, Puerto Rico declared a public health emergency
Phases of Symptomatic Dengue Fever (2-7)
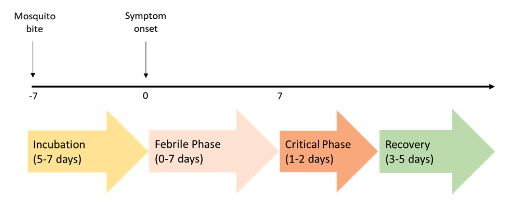
Approximately 40-80% of infections are asymptomatic during an incubation period. Generally, symptomatic dengue begins after an incubation period of 5-7 days (range 3-10 days) after a mosquito bite, and has a 3-phase course: febrile, critical, and recovery. Symptomatic dengue presents a mild-to-moderate, nonspecific, and acute febrile illness (having a fever).
Febrile Phase: Typically, the fever lasts about 7 days. Patients at this phase can spread dengue, and they should avoid mosquito bites to reduce risk for further community transmission by mosquito bites. Patients may have additional symptoms including skin redness or red patches on the skin, severe headache, pain behind the eyes, severe joint and muscle pain, upset stomach, nausea, vomiting, easy bruising and bleeding. Warning signs of progression to severe dengue usually occur in the late fever phase when the temperature drops to below 100.4°F (defervescence). Signs and symptoms to monitor are severe abdominal pain and/or difficulty breathing.
Critical Phase: This phase begins at defervescence and typically lasts 1-2 days. Most patients improve, but those with substantial bleeding progress to severe dengue could have continuous vomiting, severe abdominal pain, fluid in the chest and belly, fast breathing, low blood pressure, and/or bleeding. Patients with severe dengue may have life-threatening symptoms including troubling breathing, severe hemorrhaging, damage to organs, and/or dengue shock syndrome.
Recovery Phase: This phase may last 3-5 days. It’s possible that patients who have passed the febrile phase can recover without going through the critical phase. During this phase, patients gradually improve and symptoms are diminished including improved appetite, increased urination, ameliorated gastrointestinal symptoms, and stabilized bleeding problems. Patients may experience skin rashes, itchy skin, slow heartbeat, and/or altered level of consciousness.
Clinical Classification of Dengue (2-7)
The World Health Organization classifies symptomatic dengue as dengue without warning signs, dengue with warning signs, and severe dengue.
Dengue without warning signs–there are more than 2 clinical symptoms in a febrile person. Symptoms include fever, nausea, vomiting, rash, aches and pains, positive tourniquet test (a marker of capillary fragility), and leukopenia, etc.
Dengue with warning signs–patients should be monitored closely. Symptoms include abdominal pain or tenderness, persistent vomiting, fluid accumulation, mucosal bleeding, lethargy, restlessness, postural hypotension, and liver enlargement
Severe Dengue–fewer than 5% of dengue patients develop severe dengue. Untreated severe dengue may have a mortality rate of 10 - 20%. However, with appropriate supportive care, the mortality rate can be reduced to ~ 1%. Untreated severe dengue may cause other complications including liver injury, cardiomyopathy, pneumonia, orchitis, oophoritis, seizures, encephalopathy, and encephalitis. Symptoms include shock or respiratory distress due to severe plasma leakage, severe bleeding, severe organ impairment (e.g., hepatitis), impaired consciousness, or heart impairment.
Diagnosis (2-7)
Special blood tests are available to check for the DENV infection.
For people with symptoms ≤ 7 days after symptom onset, one of these test combinations are used:
A nucleic acid amplification test (NAAT) (e.g. RT-PCR) and an IgM antibody test
A non-structural protein 1 (NS1) antigen test and an IgM antibody test
A positive NAAT or NS1 test can confirm DENV infection
A positive IgM test can detect recent or current DENV infection
For people with symptoms > 7 days after symptoms onset, IgM antibody test is recommended to detect antibody formation against DENVs
Treatment (2-7)
There is no specific medicine to treat dengue. Depending on the clinical symptoms and other factors (age, current and past health condition, and patients’ preferences), some patients might need only supportive care, whereas patients with severe dengue might require hospitalization. Treatment options may include:
Acetaminophen to reduce fever and pain. (Do not take aspirin, ibuprofen, nonsteroidal anti-inflammatory drugs (NSAIDs), and other anticoagulants as these medications may increase risk of bleeding.)
Intravenous fluid therapy for patients with plasma leakage
Rest
Hydration.
Watch for warning signs of severe dengue as fever goes away: abdominal pain/tenderness, frequent vomiting, bleeding from the nose or gums, vomiting blood, blood in the stool. (Severe dengue is a medical emergency).
Blood transfusion for patients with consistent bleeding.
Prevention (2, 3)
There is also no vaccine to prevent dengue fever. An FDA-approved vaccine is available only for people ages 9 – 16 who have had previous dengue fever confirmed by a test and who live in areas where dengue fever is prevalent. The vaccine is not approved for use in US travelers. The best protection is to prevent mosquito bites. If you are traveling to an area with high levels of dengue fever, you should observe precaution before, during, or after your trip.
Review country-specific travel recommendations (https://wwwnc.cdc.gov/travel), health notices, and warnings.
Visit a travel clinic (https://wwwnc.cdc.gov/travel/page/find-clinic) or healthcare provider for pre-travel medical care.
Pack acetaminophen (also known as paracetamol outside of the US) to manage fever and pain.
Use an EPA-registered insect repellent on skin and clothing.
Stay in places with air conditioning and with window/door screens.
Use a mosquito net around the bed if a screened place is not available or if sleeping outdoors.
Wear loose-fitting, long-sleeved shirts and pants.
Monitor your health in the 3-10 days following your trip for any symptoms, and contact your doctor if any are observed.
Conclusion
Dengue fever is serious. It is transmitted by mosquito bites and can cause severe flu-like symptoms. Generally, it’s treated with bed rest and fluids. When traveling to areas where DENV is common, avoid mosquito bites by using proper protection. If you experience a fever within 2-3 weeks of traveling to a dengue-affected area, contact your doctor.
Dr. Young Ju is a Ph.D and Associate Professor of Human Nutrition, Foods, and Exercise at Virginia Tech.
References
CDC. Increased Risk of Dengue Virus Infections in the United States. https://emergency.cdc.gov/han/2024/han00511.asp
WHO. Dengue Global Situation https://www.who.int/emergencies/disease-outbreak-news/item/2024-DON518
CDC. Dengue. https://www.cdc.gov/dengue/index.html
National Library of Medicine. Dengue Fever. https://www.ncbi.nlm.nih.gov/books/NBK430732/
Saeed & Asif. Chapter 2 - Dengue Virus Disease; the Origins. Dengue Virus Disease from Origin to Outbreak. Academic Press, 2020, pp 9-16
Mayo Clinic. Dengue fever. https://www.mayoclinic.org/diseases-conditions/dengue-fever/symptoms-causes/syc-20353078
Johns Hopkins Medicine. Dengue fever.https://www.hopkinsmedicine.org/health/conditions-and-diseases/dengue-fever
This information is provided for your reference and you use at your own risk; you should rely on your medical professional for medical advice.